Click the link below to download the PDF copy:
How CRP inflammatory marker could contribute to the monitoring of COVID-19?
Focus Note #2 : Inflammatory Marker
Click the link below to download the PDF copy:
How CRP inflammatory marker could contribute to the monitoring of COVID-19?
Focus Note #2 : Inflammatory Marker
Published April 8, 2020
Summary
This global epidemic of coronavirus that we are currently experiencing, need an over view on the biological markers that allow the monitoring of COVID-19 disease. After a synopsis of the clinical characteristics and the management of patients, we propose a literature review of the diagnostic tests which include molecular and serological diagnosis. The aim of this document is to show the biological markers involved in screening, triage and prognosis, which involves white blood cells, platelets, Ddimer, CRP and fibrinogen. While acknowledging that these parameters are not exhaustive, they nonetheless represent essential biological markers for the management of this epidemic. (To read the full article, click here.)
Christian Siatka, Marion Eveillard, Jun Nishimura, Christophe Duroux and George Ferrandi
Several biomarkers have been observed to be abnormal in COVID-19 infected patients and the relevance of identifying them resides on decreasing the possibility of misdiagnosing severe COVID-19 (36) and to provide more insightful information for better management of COVID-19 patients. Many cohorts of different populations have been reported, principally from China, showing abnormal laboratory assessments consisting mainly of complete blood count, liver and renal function, biochemical and coagulation testing, inflammatory factors, and others.
Hematology Parameters
Different authors have published findings regarding the effect on hematology parameters in COVID-19 infected patients. The vast majority concur on an unbalanced white blood cells panel (37).
White Blood Cells
In the hematological panel, a study that evaluated 1099 positive COVID-19 samples showed on admission and 83.2% of lymphocytopenia (fewer than 1500 cells per mm 3) and leukopenia in 33.7% (16), other authors support these observations especially lymphocytopenia in severe patients (seefigure 1) (38) (39) (40) (41) (42) (43) and others reported normal levels of leukocytes (44) (45). Furthermore, neutrophils seem to increase according to the severity of the COVID-19 (14) (17). In a study with 13 patients admitted to ICU and 28 to non-ICU care, the medians of the neutrophil count were 10.6 and 4.4 × 109/L, respectively (14). Consequently, due to a significant decrease of lymphocytes and neutrophil increase, the neutrophil-lymphocyte ratio, along with the age of patient, has been suggested as a combined parameter to evaluate the severity of patients with pneumonia caused by COVID-19 for improving risk stratification and management (45) (36).
Figure 2: Lymphocyte mean count in non-severe and severe patients from different authors. The definition of severity varies slightly among references. In all the references inspected, a decrease of lymphocytes was observed in association of COVID-19 severity. The numbers inside the parenthesis are the numbers of non-severe and severe patients per study.
Platelets
A meta-analysis was performed of platelet number in COVID-19 patients with or without severe disease and odds ratio (OR) of thrombocytopenia for severe form of COVID-19 (42). The pooled analysis revealed that platelet count was significantly lower in patients with more severe COVID-19. A subgroup analysis comparing patients by survival, found an even lower platelet count was observed with mortality. In this study, a low platelet count was associated with over fivefold enhanced risk of severe COVID-19 (42). The low platelet count could be associated with increased risk of severe disease and mortality in patients with COVID-19.
CRP
Although C-reactive protein (CRP) does not normally elevate significantly in mild viral respiratory infections, levels have shown to increase in severe cases of avian influenza H1N1 and H7N9, and during the SARS epidemic in 2003. A similar significant increase of CRP has also been reported in COVID-19 patients. COVID-19 can cause mild or highly acute respiratory syndrome with consequent release of pro-inflammatory cytokines, stimulating macrophages and hepatocytes to produce CRP in higher amount.
CRP is the inflammatory marker that has more relevance than other inflammatory markers for assessing the severity of COVID-19 from current literature review (50) (36) (51). For example, in 56.4% of the non-severe cases had a CRP value higher or equal than 10 mg/L, however, in severe cases, the percentage was 81.5%. In comparison, non-severe and severe cases with PCT ≥ 0.5 ng/ml had a corresponding 3.7% and 13.7% of the samples, respectively (16). In a study comparing 82 non-severe patients and 56 severe patients, the p-values of CRP and pro-calcitonin (PCT) medians were less than 0.001 (52), however, in other articles it has been reported PCT having a normal level (48).
Figure 4: CRP mean count in non-severe and severe patients of different authors. The definition of severity varies slightly among references. In all the references inspected, an increase of CRP was associated with COVID-19 severity.
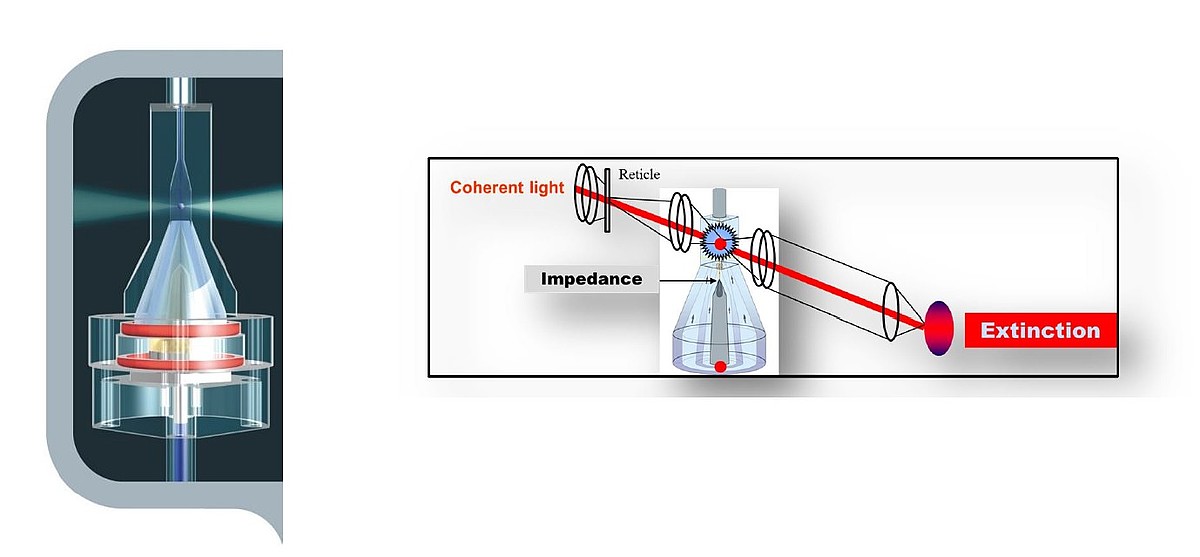
2.1. The infectious screening with CRP hematology systems
As major hematology IVD specialist, HORIBA Medical is capable to deliver hematology solutions to clinical labs in the world. The unique CRP hematology products line consist of automated testing systems designed to perform Full Blood Count (FBC) analysis combined with C-Reactive Protein assay with Microsemi CRP and Pentra MS CRP.
Dedicated to pediatrics, care units, emergencies, physician offices (POLs)
⇨ for Complete Blood Count : Red Blood Cells : RBC, HGB, HCT, MCV, MCH, MCHC, Platelets : PLT, MPV, PDW, PCT 3 Diff WBC for Microsemi CRP : WBC, LYM # %, MON # %, GRA # % |
Latex agglutination at 660 nm CRP : [ Linearity Range ] CRP whole blood [ 0,2 – 200 mg/L ] |
⇨ for Differential Leucocytes Count on Pentra MS CRP 5 Diff WBC : WBC, LYM # %, MON # %, NEU # %, EOS # %, BAS # %, LIC # %, ALY # % |
The ratio between Neutrophil Count and Lymphocytes count can be used when combined with other parameters as an indicator of inflammation and infection.
Recent Chinese publication on COVID-19 monitoring highlight the clinical value of NLR when combined with age criteria as an early indication of severe illness.
On Pentra MS CRP, this ratio can be calculated from Neutrophils and Lymphocytes absolute counts of the results report and hence provide the users with the NLR value in the final FBC report.
On Microsemi CRP, the Neutrophils are included into the Granulocytes count. Important decrease of Lymphocytes count could significantly decrease the Granulocytes population and hence provide closed clinical value of a Granulocytes-To-Lymphocytes ratio (GLR).
The GLR will be available on next version of Microsemi CRP.
● The Microsemi CRP and Pentra MS CRP are very easy to use in a POCT setting during this time of crisis and can be used with minimal training by nurses or other non-laboratory staff.
● Ideal for micro samples:
Capillary and venous blood sample without pre-treatment
2 analysis modes : CBC mode on whole blood
CBC+CRP mode on whole blood and serum
● Through a very user friendly interface and software the identification is easy managed with bar code reading.
● The CRP reagents are ready to use liquid reagents in cassettes.
All-in-one 3 reagents in single cartridge
● The CRP calibration is automatic since barcoded master curves are provided with very upload ease.
● The CRP solutions are capable to provide fast screening of microbial infection and predictive diagnosis of infectious diseases.
Due to the huge flow of patients in worldwide medical centers, the physicians need a near patient solution allowing a rapid triage and ease of operation for the users (nurses, untrained staff…):
The hematology analyzers such as Microsemi CRP and Pentra MS CRP are capable to provide infectious screening by combining enhanced technologies and providing relevant biological markers. These analyzers are designed to be easy implemented in care units with safe handling under biohazard control.
More and more combination of parameters are found to be relevant for screening and monitoring infectious diseases.
Infectious diseases can not only be monitored with dedicated infectious diagnostics tools but also biological testing systems are more and more suitable for delivering significant markers to help and contribute to their monitoring.
Tiene alguna pregunta o solicitud? Utilice este formulario para ponerse en contacto con nuestros especialistas.