Click the link below to download the PDF copy:
How biological markers could contribute to the monitoring of COVID-19?
Focus Note #1 : Hematology Biological Markers
Click the link below to download the PDF copy:
How biological markers could contribute to the monitoring of COVID-19?
Focus Note #1 : Hematology Biological Markers
Published April 8, 2020
Summary
This global epidemic of coronavirus that we are currently experiencing, need an over view on the biological markers that allow the monitoring of COVID-19 disease. After a synopsis of the clinical characteristics and the management of patients, we propose a literature review of the diagnostic tests which include molecular and serological diagnosis. The aim of this document is to show the biological markers involved in screening, triage and prognosis, which involves white blood cells, platelets, Ddimer, CRP and fibrinogen. While acknowledging that these parameters are not exhaustive, they nonetheless represent essential biological markers for the management of this epidemic.
Christian Siatka, Marion Eveillard, Jun Nishimura, Christophe Duroux and George Ferrandi
Several biomarkers have been observed to be abnormal in COVID-19 infected patients and the relevance of identifying them resides on decreasing the possibility of misdiagnosing severe COVID-19 (36) and to provide more insightful information for better management of COVID-19 patients. Many cohorts of different populations have been reported, principally from China, showing abnormal laboratory assessments consisting mainly of complete blood count, liver and renal function, biochemical and coagulation testing, inflammatory factors, and others.
Hematology Parameters
Different authors have published findings regarding the effect on hematology parameters in COVID-19 infected patients. The vast majority concur on an unbalanced white blood cells panel (37).
White Blood Cells
In the hematological panel, a study that evaluated 1099 positive COVID-19 samples showed on admission and 83.2% of lymphocytopenia (fewer than 1500 cells per mm 3) and leukopenia in 33.7% (16), other authors support these observations especially lymphocytopenia in severe patients (seefigure 1) (38) (39) (40) (41) (42) (43) and others reported normal levels of leukocytes (44) (45). Furthermore, neutrophils seem to increase according to the severity of the COVID-19 (14) (17). In a study with 13 patients admitted to ICU and 28 to non-ICU care, the medians of the neutrophil count were 10.6 and 4.4 × 109/L, respectively (14). Consequently, due to a significant decrease of lymphocytes and neutrophil increase, the neutrophil-lymphocyte ratio, along with the age of patient, has been suggested as a combined parameter to evaluate the severity of patients with pneumonia caused by COVID-19 for improving risk stratification and management (45) (36).
Figure 2: Lymphocyte mean count in non-severe and severe patients from different authors. The definition of severity varies slightly among references. In all the references inspected, a decrease of lymphocytes was observed in association of COVID-19 severity. The numbers inside the parenthesis are the numbers of non-severe and severe patients per study.
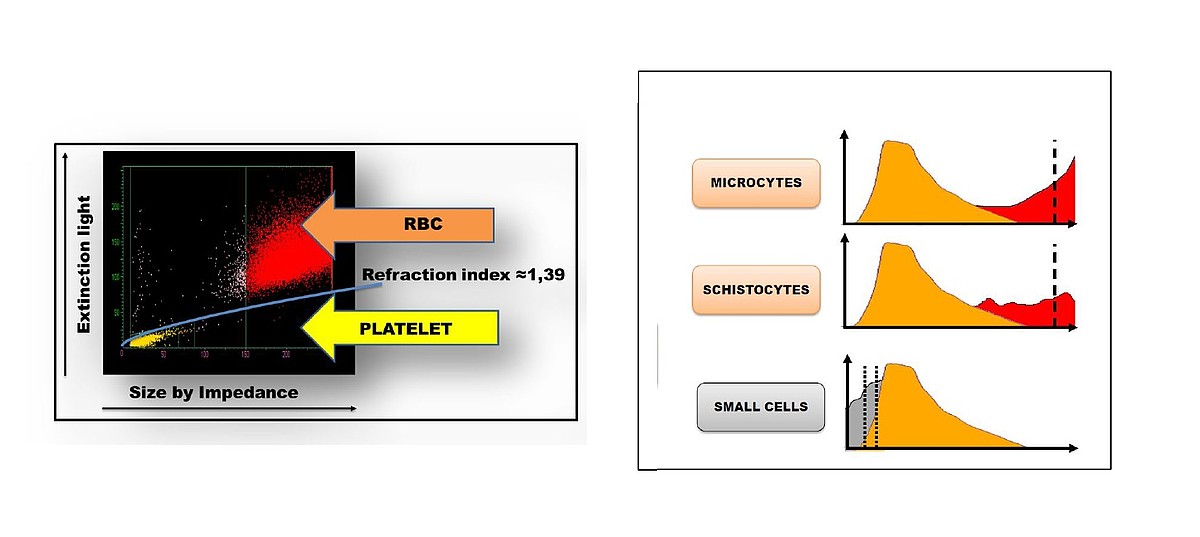
Platelets
A meta-analysis was performed of platelet number in COVID-19 patients with or without severe disease and odds ratio (OR) of thrombocytopenia for severe form of COVID-19 (42). The pooled analysis revealed that platelet count was significantly lower in patients with more severe COVID-19. A subgroup analysis comparing patients by survival, found an even lower platelet count was observed with mortality. In this study, a low platelet count was associated with over fivefold enhanced risk of severe COVID-19 (42). The low platelet count could be associated with increased risk of severe disease and mortality in patients with COVID-19.
As major hematology IVD specialist, HORIBA Medical is capable to deliver hematology solutions to clinical labs in the world. The new Yumizen® hematology products line consist of automated testing systems designed to perform Full Blood Count (FBC) analysis in small labs with Yumizen H500 and Yumizen H550; and in big labs with Yumizen H1500 and Yumizen H2500.
*HORIBA Evolutive Laboratory Organization
⇨ for Complete Blood Count : Red Blood Cells : RBC, HGB, HCT, MCV, MCH, MCHC, Platelets : PLT, MPV, PDW, PCT, P-LCC*, P-LCR* |
⇨ for Differential Leucocytes Count White Blood Cells : |
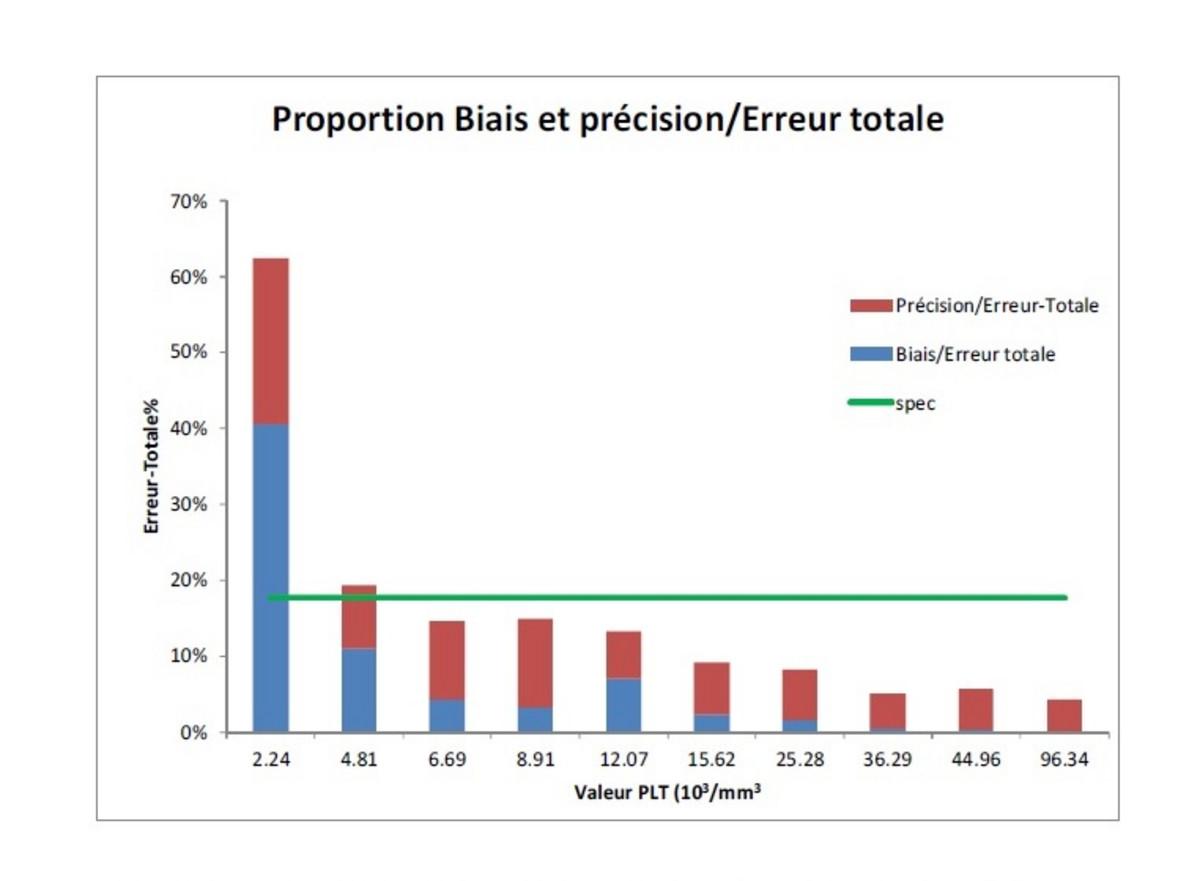
On new Yumizen analyzers range, the PLT measurement by impedance has been enhanced in such way to reach the lowest acceptable concentration _ Limit Of Quantification (LOQ) _ below 10.109/L fitting the clinical threshold to help the clinicians to take the appropriate decision of blood transfusion.
Clinical Assessment of LOQ on Yumzien H500 & Yumizen H550
| The LOQ has been obtained with an imprecision claim (total error) of 17,7% as per the clinical standard of Gröner & Simpsons |
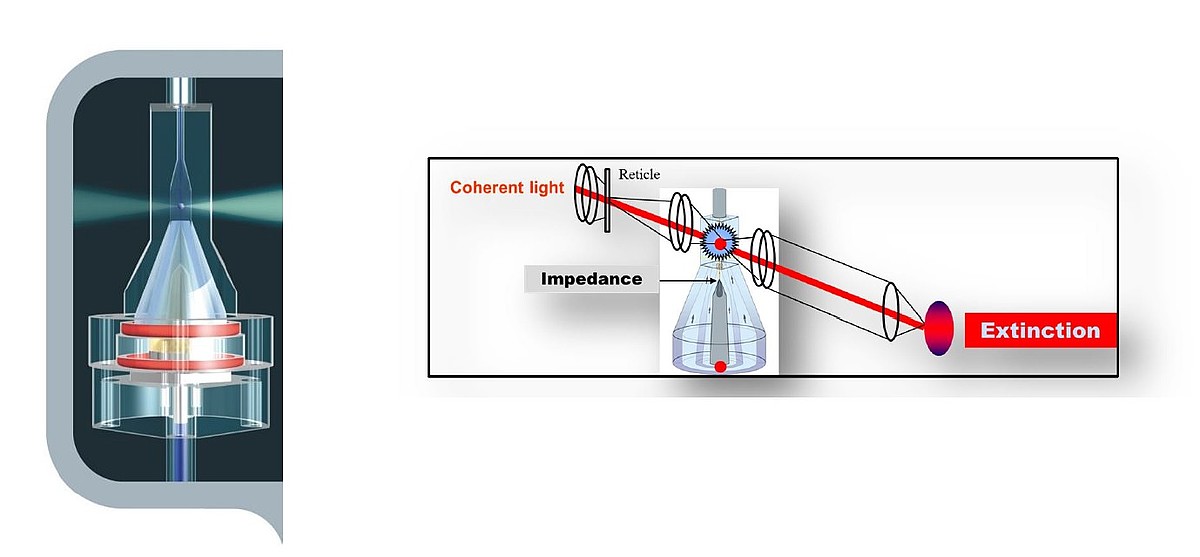
On Yumizen H1500 and Yumizen H2500, an alternative measurement of Platelets can be performed from optical extinction technology. The called PLTox parameter can be obtained by reflex testing and especially useful in case of platelets interferences.
The WBC count is ensured trough different measurements technologies on the different HORIBA Medical hematology analyzers available:
| WBC Measurement | Impedance CBC/HGB Channel | Impedance Baso Channel | Optical LMNE Channel | WBC & Diff Parameters |
| Micros range | ✓ | WBC, 3 Diff | ||
| Pentra range | ✓ | ✓ | ✓ | WBC, 5 Diff |
| Yumizen H500/550 | ✓ | WBC, 6 Diff | ||
| ✓ | ✓ | ✓ | TNC, WBC, 8 Diff |
Detection of WBC abnormalities in term of size and content is perfectly detected with great sensitivity and specificity. Thanks to the technology of double hydro-focalization system sampling (DHSS®), the Yumizen systems are able to give you the size of cells, the content and also the distribution per sub leucocytes population: Lymphocytes, Monocytes, Neutrophils, Eosinophils and Basophils. The clusters of each population are automatically surrounded with a specific attention around Lymphocytes population with LN flags, ALY,…
The HORIBA Medical technology embedded in Yumizen analyzers are particularly powerful for detecting inflammations or infections. It also helps you monitor therapies – elevated white blood cell counts going down can show therapies are working.
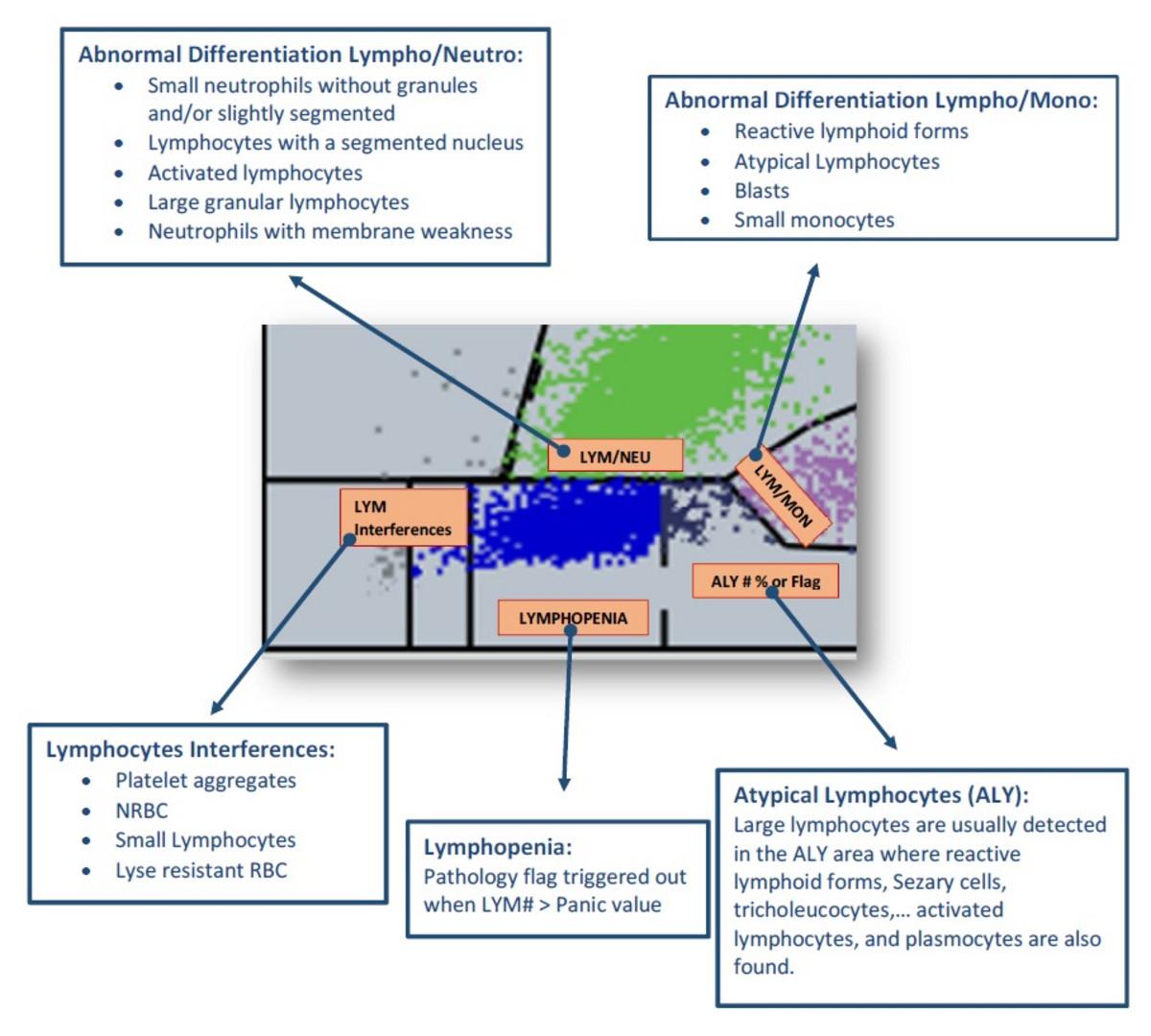
Current LMNE Matrix for Differential WBC on Yumizen range
The HORIBA Medical hematology analyzers integrate in the DIF mode sub leucocytes population in a specialized area to count Lymphocytes (LYM). It is of particular interest for samples with detected abnormalities either on cells enumeration or cells morphologies.
Lymphocytes are very small, round shaped cells with a condensed cytoplasm and a large nucleus. These cells are normally positioned in the lower part of the Y-axis, as well as in the left part of the X-axis, of differential matrix, because of their small size.
An expert flagging system is capable to trigger out flags and alarms in case of pathological abnormalities in order to provide comprehensive diagnosis help to clinicians for validating their hematology results.
The ratio between Neutrophils count and Lymphocytes count can be used when combined with other parameters as an indicator of inflammation and infection.
Recent Chinese publication on COVID-19 monitoring highlight the clinical value of NLR when combined with age criteria as an early indication of severe illness.
This ratio can be now set up on Yumizen P8000 middleware of Yumizen H1500/2500 and hence provide the users with the NLR value in the FBC report.
The NLR will be also available on next version of Yumizen H550, and then, on future version of Yumizen H500.
The hematology analyzers such as Yumizen are capable to deliver reliable hematology diagnosis by combining enhanced technologies and providing multiple parameters; from small care units to much bigger laboratories centers. More and more sophisticated flagging system are implemented to help the clinicians to interpret cells abnormalities and provide safe pathological diagnosis.
Infectious diseases cannot be only monitored with dedicated infectious diagnostics tools but also biological testing systems are more and more suitable for delivering significant markers to help and contribute to their monitoring.
Masz pytania lub prośby? Skorzystaj z tego formularza, aby skontaktować się z naszymi specjalistami.