
Strangles is one of the most common infectious diseases in horses, but managing it presents a multifaceted challenge: From diagnosis, to treatment, quarantine and hygiene measures, tackling suspected and confirmed strangles cases can be a headache for veterinary professionals, plus a significant expense for horse owners. From the largest yards to small stables, rapid testing, biosecurity and vaccination can all be valuable in the effective handling of the disease.
For veterinary professionals, strangles can be a challenging disease to identify and diagnose. Early-stage infection can be asymptomatic, while the clinical presentation of pyrexia, nasal discharge and swollen lymph nodes can resemble other respiratory illnesses. Furthermore, commonly used tests for strangles can be ambiguous and difficult to interpret. Following a positive strangles diagnosis, implementing effective isolation and management of infected individuals is key to preventing the spread of disease, adding logistical complications, especially for larger yards and those where there may be frequent movement of animals.
For horse owners and carers, strangles comes with significant financial implications – the costs associated with testing, quarantine and lost days of work can quickly escalate. While strangles outbreaks often spark panic in horse owners, the majority of cases are mild, and the condition has a very low mortality rate. If left unmanaged however, the disease can rapidly spread through the equine community, leading to increased animal morbidity and causing disruption and further economic loss for owners.
To help tackle the challenges faced by veterinary professionals in managing strangles cases, HORIBA UK Veterinary invited RCVS recognised specialist in equine medicine, Dr Mark Bowen FRCVS, to share his insights and experience as part of its successful ongoing CPD webinar series. The webinar, titled “Keeping Strangles at Bay” included some valuable tips on best practices for disease diagnosis, case management and treatment.
In this article, we will cover some of the key highlights from the webinar, and provide practical advice, including how rapid in-house testing can help support clinical decision making and limit the financial impact of strangles outbreaks.
Strangles, caused by the bacterium Streptococcus equi (S. equi), is a highly contagious infection of the equine upper respiratory tract. The disease is most commonly observed in younger horses (<5 years), with many individuals developing long-term natural immunity following S. equi infection. The infection takes hold in the nasopharyngeal epithelial cells, and migrates through the mucous membranes in the nose and mouth. S. equi then spreads to the lymphatic system and lymph nodes, where a severe inflammatory response causes abscesses to form that can eventually rupture (Figure 1). Keeping the pathogenesis of strangles in mind is important since the location and stage of infection can impact upon the sensitivity and reliability of diagnostic tests.
 |  |
Figure 1: Lymph node swelling and abscessation characteristic of strangles
The severe lymph node swelling observed in strangles cases is exacerbated by the bacteria forming protective hyaluronic acid capsules, rendering them resistant to phagocytosis. As neutrophils migrate to the locus of infection, antiphagocytic factors such as the S. equi SeM and Mac proteins add further resistance, causing the white blood cells to accumulate as more and more are recruited by the immune system to combat the infection. As the lymph nodes inflame, the swelling compresses upon the upper respiratory tract – from this, the name strangles is derived. Although lymph node abscessation is most commonly observed in the submandibular and retropharyngeal nodes, it can also manifest in the parotid and cranial cervical nodes.
As well as strangles caused by S. equi, illness can be brought about by infection with another pathogenic strain, Streptococcus zooepidemicus. While S. zooepidemicus was once thought of as a relatively harmless, commensal species, infection can be just as severe as that caused by S. equi, and as the name may suggest, it brings a greater threat of zoonosis and infection in other species. As such, it is highly recommended to use PPE around suspected strangles cases, and to strictly isolate suspected infected individuals from other animals and immunocompromised people who carry an increased risk of infection from either strain. Although used less now, due to advances in diagnostic techniques, differentiating between the two pathogenic strains is possible through traditional agar-based bacteriology. When cultured on agar, S. equi displays beta-haemolysis with colonies manifesting in a distinct mucoid appearance (Figure 2). S. equi exhibits poor adherence to the agar versus S. zooepidemicus, and can be easily moved by shaking the plate. Another characteristic of S. equi is the unique yeast-like smell that it produces, which is powerful in comparison to the S. zooepidemicus variant.
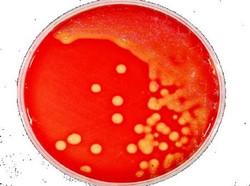
Figure 2: An agar plate containing cultured S. equi. Colonies display a distinct mucoid appearance.
In acute strangles cases, the initial symptoms of pyrexia and lethargy present from approximately 3 days following exposure to S. equi. The characteristic pharyngitis and lymph node abscessation develops 1-3 weeks post-infection, most commonly presenting in the submandibular and retrophayngeal areas, although the parotid, cranial cervical and retrobulbar lymph nodes can also be affected. Abscesses will typically rupture around seven days after developing, although it could take up to four weeks.
Abscesses can either rupture externally, with discharge escaping through the skin, or internally into the airways or guttural pouch, risking a much longer-term grumbling condition and long-term strangles carrier status for the individual. Infected horses regularly develop a cough, and produce a yellowish nasal discharge, possibly carrying the characteristic S. equi smell. General inflammation in the airways caused by strangles can lead to respiratory tract obstruction, therefore practitioners should exercise caution if considering sedation and take precautions in case of causing the patient to collapse. In severe cases, dysphagia and even loss of pharyngeal function may occur, giving a poor prognosis for these animals.
From the first exposure to S. equi, to the lymphatic system becoming inoculated may take up to 3 days. The first clinical signs of pyrexia and lethargy onset after an incubation period of potentially up to 2 weeks, with a short window of around 24 hours between developing symptoms and the onset of bacterial shedding – at which point the individual is highly infectious to other horses. Bacterial shedding may even occur before any clinical signs are noticed, meaning that recently infected animals present a significant risk. Typically, after 3 weeks, most individuals will have developed an immune response, and after 6 weeks should have a complete resolution of clinical signs.
Data shows that in somewhere around 10% of cases however, S. equi infection is not resolved as swiftly. In particular, bacteria that reside in the guttural pouch can cause an infected individual to develop long-term carrier status. In these cases, the horse may have episodes of intermittent shedding for years, although showing no clinical signs. These cases are a particular problem for veterinary professionals, yard and horse owners, as they can easily go unnoticed.
When considering strangles diagnosis, it is important to know when confirmation is necessary. In many cases, confirmatory diagnostic tests for strangles are not necessary – and instead, erring on the side of caution with patient management is recommended. If a horse looks like it has strangles, it is best to assume that the individual has the disease, and treat them as such.
Diagnostic tests may be helpful to confirm the presence of S. equi or S. zooepidemicus. However, if a test comes back positive for either strain, the course of action is the same – the individual should be isolated immediately.
There are a number of options when it comes to diagnostic testing for strangles. The test selected should take into account the stage of infection – for example, a nasal swab would be ineffective in a recently-exposed horse since the infection would not have had time to spread through the mucosa into the nasopharyngeal tissues, and would also be less likely to detect a carrier, where a guttural pouch wash is used. Mark also gave some handy practical tips for guttural pouch endoscopy and emphasised that the more the technique is practised, the easier it becomes. The following are some of the most commonly implemented tests:
Serology is an effective approach to detect exposure to S. equi, with protein targets peaking at around 5 weeks post infection or exposure. Serology testing for strangles differs between the UK and USA, in that the protein target tested for in the USA is SeM, while in the UK, A/C antigens are more commonly targeted, as it is thought to give better differentiation between S. equi and S. zooepidemicus.
Whichever serology target is used, it can be reliably detected by ELISA, a reasonably fast and inexpensive test. However, while an effective method of detecting exposure and identifying strangles at individual and herd level, serology cannot differentiate between recent exposure and active disease.
This approach is reliant upon collecting a sample from the locus of infection. A fine needle aspirate can be taken from a swollen lymph node (sedation recommended), a nasopharyngeal swab or wash is indicated in the acute stage of infection, but is not helpful when testing for carrier status, where guttural pouch lavage is indicated.
Analysis of the sample taken using PCR is the current gold standard, as it provides the best possible speed and specificity for detecting S. equi, with in-house systems offering results in under two hours, however, samples may also be inoculated in agar for growth and microbiological analysis. It should be noted that nasopharyngeal swabs may only be appropriate in individuals with visible nasal discharge, and any bacterial sampling can only be successful in areas with current visible infection.
Managing strangles outbreaks requires careful isolation of infected individuals, and treatment will often be necessary to speed up recovery. No matter whether a horse is ill with S. equi or S. zooepidemicus, an out-of-control infection can become life-threatening. For horses with swollen lymph node abscesses, poulticing and draining the pus is recommended, alongside NSAIDs like meloxicam, and in severe cases, antimicrobial treatment. There are a number of myths surrounding antimicrobial treatment of strangles, for example some believe that antimicrobials may prolong the resolution of abscesses, or that it may be an obstacle to the horse developing natural immunity. There is no evidence to support these myths.
The use of antibiotics to treat strangles can divide opinion. Careful consideration must be given to each individual case, in relation to clinical signs and environment. Information for prescribing and the responsible use of antibiotics, bearing in mind the effects of antimicrobial resistance, is available on the BEVA ProtectME guidance [1]. While most owners faced with strangles will be keen to employ antibiotic treatment, it is not always essential, and cases can often be managed with NSAIDs alone. Nonetheless, there are situations where the use of antibiotics is justified, and sometimes essential:
Antibiotics are not to be used as a metaphylactic measure – this is an ineffective way of generating herd protection, as it can reduce the overall effectiveness of antibiotics, and facilitates antibiotic-resistant strangles strains. Furthermore, many horses who come into contact with S. equi, will develop natural resistance without becoming ill.
When dealing with a strangles outbreak, implementing effective isolation and quarantine of infected individuals is absolutely essential to curb the spread of the disease. Firstly, all movement of horses off yard should be halted – a measure that should remain until 3 weeks past the resolution of clinical signs, plus a negative PCR test from all clinical carriers. Where possible, unwell horses should be immediately isolated in a separate, well-ventilated area, with water troughs regularly emptied and cleaned. Although these measures will no doubt be unpopular with owners, and particularly on large sites, isolation is crucial to managing strangles outbreaks.
Stratifying risk into a “traffic light” system of groups can help the navigation of strangles quarantine. Green would represent disease-free horses, while amber is horses that have come into contact with a strangles patient, and finally red is for those with clinical signs of disease. If caught early enough, the green disease-free horses can be isolated from the rest of the herd, and may have a chance of remaining healthy and leaving the yard earlier. This is reliant upon the horses providing negative tests, and carrier-free status.
Administering strangles vaccines can decrease the severity and frequency of outbreaks, and help to build immunity in a herd. Strangvac (Dechra) is a newly-developed protein-based vaccine which is shown to be a highly effective prophylactic measure when implemented as per the manufacturer’s guidelines. These vaccines stimulate the horse's immune system to produce antibodies against S. equi, helping them mount a more effective defence if exposed to the pathogen.
Where a substantial portion of the horses in a herd are vaccinated, the overall transmission of the disease is greatly reduced. Consequently, vaccinated horses are less likely to develop clinical symptoms if exposed, and the likelihood of severe complications and fatalities associated with strangles is significantly diminished.
It has been noted that a proportion of horses develop transient side effects to the Strangvac vaccine, such as injection site swelling and lethargy. In addition, 2 doses are required before immunity is developed. As such, it is recommended to implement vaccination to avoid disruption to schedules and events. While owners may be reluctant to get on board with another vaccination, protecting their yard in this way can limit the runaway costs of a strangles outbreak, should one occur. Booster vaccinations as per the data sheet will be required to ensure ongoing immunity.
As we have seen, strangles is a disease that requires a multifaceted approach to manage the complexities of disease presentation, testing, treatment and prevention. Keeping a herd disease-free can be possible, but it does take a substantial amount of planning and work to succeed, especially for yards that have regular arrivals and horses mixing at competition days. As well as vaccination, some of the most important aspects to strangles prevention rely upon assessment of potential carriers, careful management of horses that move on and off the yard and regular testing including herd serology to catch cases as early as possible. Here are some of the top best practices for keeping free from strangles:
Ensure that good biosecurity is observed on and off the yard, especially when horses are handled by multiple people. Hand washing or sanitising facilities should be available and equipment should be clean and not shared.
As highlighted above, vaccination can be a highly effective way to protect a herd. By building immunity and preventing animals from developing symptoms when exposed, the overall transmission of disease can be substantially reduced. However, it is recommended that vaccination is only undertaken once the status of a herd or individual is known.
Every new arrival should be isolated for 3 weeks upon arrival to a new yard. This is irrespective of any diagnostic test results, since the horse may have been exposed to strangles during the days leading up to transit, and may develop clinical symptoms in the weeks to follow.
It can be highly valuable to determine individuals who are entirely free from disease, and to identify and treat long-term carriers, who may not show any symptoms. Any carriers can be treated appropriately, and should be re-tested after two weeks to ensure a negative test result.
Any exposure to strangles pathogens can be identified with regular testing. Knowing a horse’s baseline body temperature and monitoring regularly is a simple and cost-effective means of checking for changes in its health, via rectal temperature measurement or enhanced microchip reading. As discussed previously, serology is a highly effective way to detect exposure at the herd level, while PCR testing of suspected cases is the most sensitive method of diagnosis.
Easy to use in-house PCR platforms such as the POCKIT™ Central veterinary PCR analyser (HORIBA UK) can rapidly turn around results at any time, so that the necessary measures can be implemented in a timely manner to prevent the spread of infection. It is a highly user-friendly bench-top system that completely automates the PCR testing process for up to eight pathogens in one run, providing results directly on-site within 85 minutes (Figure 3). This enables veterinarians to rapidly make confident diagnostic and case management decisions eliminating the need to wait for external laboratory results.

Figure 3: The POCKIT™ Central bench top sample-in answer-out veterinary PCR system.
Dr Mark Bowen’s talk shone a light on the difficulties that strangles can present to veterinary professionals. From managing owner expectations, to diagnosis, treatment and isolation regimes, it is certainly not an easy task to manage a strangles outbreak. By far the most effective way to get on top of the disease, is to encourage yards to implement sound preventative measures.
Vaccination is certainly highly recommended, and an effective way of protecting the herd, but to keep a yard disease-free, regular testing should also be implemented. When a suspected case emerges, gaining reliable results as fast as possible can enable a swift isolation and treatment process that minimises the spread of disease and disruption to the yard. To achieve this, having access to easy, rapid in-house testing systems such as the aforementioned POCKIT™ Central can eliminate the potentially lengthy process of sending samples off to reference laboratories for analysis and awaiting the results.
With knowledge of the disease pathology, plus support with vaccination and rapid testing, Mark Bowen concluded that it is possible to manage strangles with confidence and to work with owners to prevent future outbreaks.