VKA therapy inhibits factors II, VII, IX, and X and causes a prolonged PT.
The impact of VKAs on clotting is indirectly assessed via the International Normalized Ratio (INR).
International Normalized Ratio for a plasma from a patient on long-term oral anticoagulant therapy is a value calculated from the prothrombin-time ratio according to the formula.
INR = (PT/MNPT)ISI
International Sensitivity Index (ISI): Thromboplastins are calibrated against a WHO international reference thromboplastin (International Reference Preparation or IRP) to give them an International Sensitivity Index or ISI.
Mean normal prothrombin time (MNPT) is the geometric mean of the PTs calculated from at least 20 fresh samples from healthy adults, including both sexes.
The WHO recommend:
- Individual samples should be collected and tested over at least three working days in order to include inter-assay variation.
- Each laboratory should determine MNPT using its own prothrombin-time system.
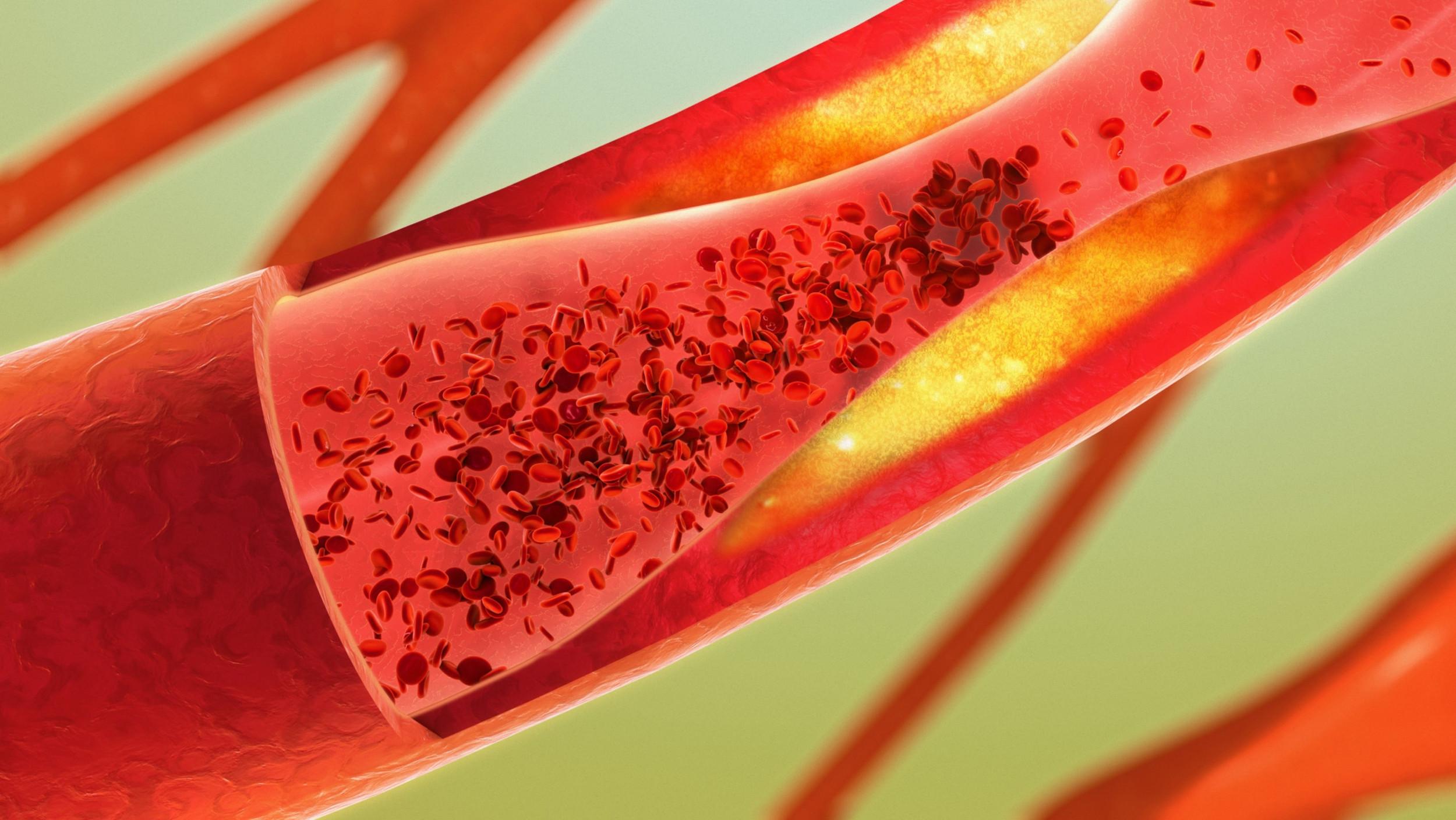
VKAs can prevent stroke or systemic embolization among patients with atrial fibrillation (AF) and can treat and prevent venous thromboembolism (VTE).
INR Normal range
The target INR is generally 2.5 and is equivalent to a range of 2.0 to 3.0
In some cases (e.g., a mechanical valve in mitral position), the target INR may be higher.
Bibliography
Tricoci P, Allen J, Kramer J, et al. Scientific evidence underlying the ACC/AHA Clinical Practice Guidelines. JAMA. 2009;301(8):831-841.
Pisters R, Lane DA, Nueuwlaat R, de Vos CB, Crijns HJ. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in atrial fibrillation: the euro heart survey. CHEST. 2010;138(5):1093-1100.
Patients who are to receive any heparin should have a baseline platelet count and platelet monitoring depending on the context.
Heparin is a commonly used medication worldwide since it is essential in the treatment and prophylaxis of thromboembolic disorders. Heparin is effective for prevention and treatment of venous thrombosis and pulmonary embolism (PE), for prevention of mural thrombosis after myocardial infarction (MI), and for treatment of patients with unstable angina and MI. Although heparin is used to prevent acute thrombosis after coronary thrombolysis, recent reports question the benefits of heparin in this setting when patients are also treated with aspirin.
It’s a sulfated polysaccharide that produces its major anticoagulant effect by inactivating thrombin and activated factor X (factor Xa) through an Antithrombin (AT)-dependent mechanism.
Two types of heparins are widely used, unfractionated heparin (UFH) and low molecular weight heparin (LMWH).
All of the anticoagulant, pharmacokinetic, and other biological differences between unfractionated heparin (UFH) and low molecular weight heparin (LMWH) can be explained by the relatively lower binding properties of LMWH. Compared with UFH, LMWHs have reduced ability to inactivate thrombin because the smaller fragments cannot bind simultaneously to AT and Thrombin.
Unfractionated heparin (UFH) is a heterogeneous mix of polysaccharide chains of variable molecular weight with a strong binding affinity to Antithrombin. They are used for both therapeutic and prophylactic therapy.
Normal ranges (Anti Xa):
To ensure optimal heparin therapy while minimizing the risk of bleeding or thromboembolic complications, refer to the heparin manufacturer’s recommendations for heparin activity.
LMWHs are derived from heparin by chemical or enzymatic depolymerization to yield fragments approximately one third the size of heparin.
Low molecular weight heparins (LMWH’s) are used to prevent and treat thrombosis.
Assays:
Gold standard for monitoring LMWH’s is anti-factor Xa (anti-FXa).
Normal ranges (Anti Xa):
To ensure optimal heparin therapy while minimizing the risk of bleeding or thromboembolic complications, refer to the heparin manufacturer’s recommendations for heparin activity.
Masz pytania lub prośby? Skorzystaj z tego formularza, aby skontaktować się z naszymi specjalistami.